Injecting Insulin
Injecting insulin is the essential part of the daily regime for many Diabetics patient. Although insulin that can be inhaled is now available and approved, the reality is that most type 1 diabetics (and type 2 diabetics who require insulin) will have to continue injecting insulin until it is more common.
Tips for Injecting Insulin
Injection sites: Insulin should be injected into the layer of fat that lies right under the skin. There are several areas on the body where you can inject your insulin. These include the:
- Abdomen (Stomach), a few inches away from belly button
- Outer thigh
- Hips
- Upper Buttocks
- Back of the arms
Painful Injection: Now a day’s super thin needles are available in the market, Insulin injection are pretty much painless, If you are finding that your injection hurt’s, Try the followings;
- Use a new needle for every injection. It’s tempting to reuse needles, but they can become dull even after just one or two injections. And the duller the needle, the more painful the injection.
- Use the thinnest needle possible. The higher the gauge, the thinner the needle.
- Use a short needle (6 mm or shorter).
- Inject insulin at room temperature.
- If you use alcohol to clean your injection site, make sure it’s completely dry before injecting.
- Relax tense muscles make the nerves in the injection area more sensitive.
- Larger doses of insulin (30 units or more) may be uncomfortable. If this is a concern, talk with your doctor about splitting your dose.
- Rubbing ice on your skin before injecting may also help.
Insulin leaking from injection sites: It’s not unusual for insulin to leak out from the injection site after you withdraw the needle. Usually, the amount that leaks out is insignificant and likely won’t affect your blood sugar levels. To minimize or avoid leakage, try the following:
- Count slowly to 10 before withdrawing the needle.
- After removing the needle, place your finger on the site for 5–10 seconds.
- If you use a pen, always remove the needle after you inject. Leaving the needle on can cause air to enter the cartridge and it will take longer to inject the insulin.
- Try injecting at a 45-degree angle rather than going straight in.
Forgetting to take you insulin: Missing even just one injection per week can raise your HbA1c level by 0.5%. How can you remember?
- Link taking your insulin with other daily habits, such as eating breakfast or brushing your teeth before you go to bed.
- Keep your insulin and supplies in a convenient place. And think about keeping supplies both at home and at work (or school).
- Don’t get distracted. Multitasking is never a good idea, especially when it comes to injections. If you’re doing too many things at once, you can easily forget to inject. Focus on the task at hand.
- Set an alarm, use sticky notes, ask your spouse to remind you — all can help you to remember.
Fear of Needles: Injection can lead to anxiety and even physical symptoms, such as light-headedness, palpitations, dry mouth, sweating, and feeling sick. Here’s what can be helpful:
- Make sure you’re using the shortest, thinnest needle that you can.
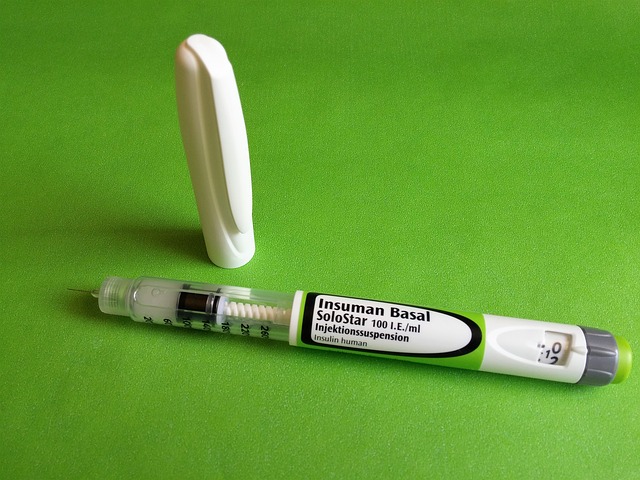
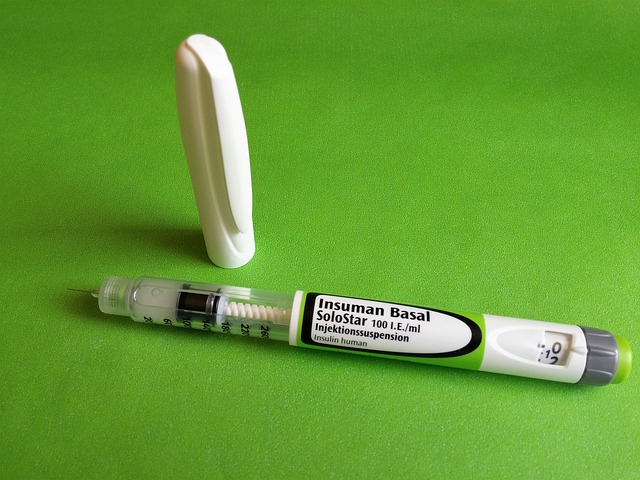
- An insulin pen may be easier for you to use than a syringe.
- Put a cold spoon or an ice cube on the injection site for a few minutes before you inject.
- Ask your doctor about using a topical anesthetic, which can numb the surface of the skin.
To read more on Patient Care, click on the link below.
Content Courtesy : Portea