Understanding Diabetes
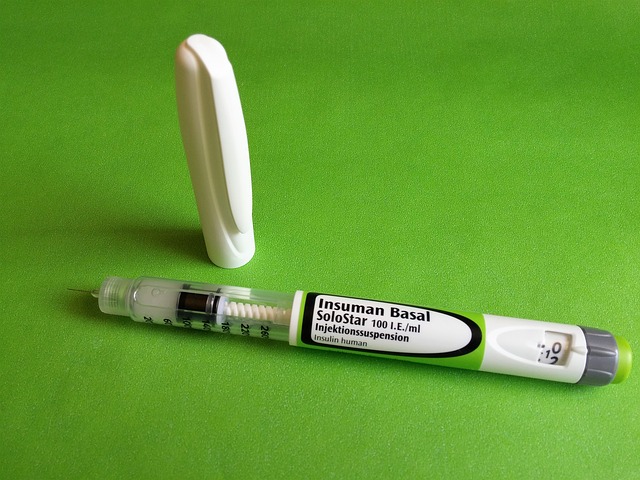
Diabetes is an endocrine disorder that elevates your blood sugar levels over a prolonged period of time. It is caused by the malfunctioning of the pancreatic cells, which produce insufficient or no Insulin. It is a chronic disorder which can be managed with right medication and healthy lifestyle.
Deeper Dive
Managing diabetes can feel overwhelming at times. However, understanding the deeper aspects can
burst many myths and shows diabetes can be managed easily. Let’s venture out different diabetes
issues and better ways to deal them.

Fluctuating Glucose Levels by Famhealth
Erratic Glucose Levels High, fluctuating or unmanageable blood glucose levels...
Checklist & Tips for Diabetics by Famhealth
Checklist with Tips For Patients Here’s a quick guide for...
Children and Diabetes by Famhealth
Children and Diabetes Kid eating candy My child has diabetes...
Just Detected with Diabetes by Famhealth
Just Detected Being diagnosed with diabetes can be an overwhelming...
Managing Diabetes
Lifestyle changes include adopting a healthy diet and exercise plan which plays a direct role in
controlling the blood glucose levels of a person living with diabetes. It is important to deal with the stress
and emotional turmoil that comes with this diagnosis and so getting the right support and
making lifestyle changes to successfully manage this condition is imperative.

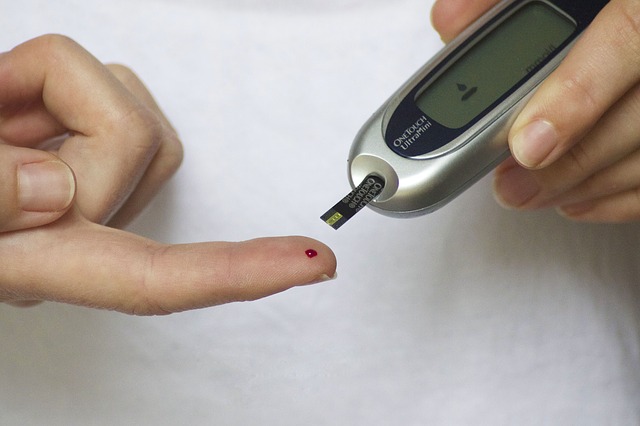
Tests for Diabetes by Famhealth
Tests for Diabetes Why are they important? With knowledge comes...
Exercise for Diabetic Patients by Famhealth
Exercise for Diabetic Patients As you may already know Diabetes...
Handy tips for people living with diabetes curated by Famhealth
Handy tips for people living with diabetes Are you tired...
The Correlation Between Diabetes And Food by Famhealth
The Correlation Between Diabetes And Food The Correlation Between Diabetes...
Self measures to prevent diabetes by Famhealth
Self measures to prevent diabetes Excess weight is the single...
Compliance and Checklist for Diabetes by Famhealth
Compliance and Checklist Compliance and Checklist for Diabetes by Famhealth...
Diabetes And Your Personality
A research conducted on 3500 patients by a school in Westminster, USA concluded that there are two major personality characteristics in the management of diabetes are the Interactive and the
Independent personality.
Happy Living
A healthy diabetes diet aids in treating and controlling blood sugar level. Though everyone requires a
balanced diet to stay healthy, diabetics need to watch out the food they eat to keep an eye on spiked
blood sugar levels. Here are some healthy eating strategies which can curb diabetes.

Diabetes Diet Options curated by Famhealth
Diabetes Diet Options Hello everyone! Here’s introducing everybody, to absolutely...
Eating Strategies for Weight Loss & Diabetes by Famhealth
7 Smart Eating Strategies To Lose Weight And Reverse Diabetes...
Diabetes-Friendly Grocery Shopping Items by Famhealth
Diabetes Friendly Grocery Shopping Items Going for grocery shopping for...
Diabetes Food Myths & Facts by Famhealth
Diabetes food myths and facts Myth: People with diabetes should...
Diabetes Friendly Recipes
An assortment of some yummy diabetic-friendly recipes are not bring down blood sugar levels, but are
a delight to eat. Here we bring you easy and quick recipe tricks and tips, which are easy and quick to cook.

Diabetes Recipe – Chiang Mai Chicken Curry by Famhealth
Diabetes Recipe – Chiang Mai Chicken Curry Nutrition FactsMakes 4...
Diabetes Recipe – Hearty Chicken Stew by Famhealth
Diabetes Recipe – Hearty Chicken Stew Preparation :25 Minutes Cooking...
Diabetes Recipe – Papaya And Coconut Smoothie by Famhealth
Papaya And Coconut Smoothie Nutrition FactsMakes 2 servings(Amount per Serving)Calories...
Diabetes Recipe – Baked Lemon Fish With Tomatoes by Famhealth
Diabetes Recipe – Baked Lemon Fish With Tomatoes Preparation :15...
Diabetes Recipe – Mediterranean Veggie Wrap
Diabetes Recipe – Mediterranean Veggie Wrap Preparation :10 Minutes Cooking...
Diabetes Recipe – Tropical Banana Freeze
Diabetes Recipe – Tropical Banana Freeze Serves: 4, Time taken:...
Related Videos On TV

Diabetes Support Groups
These inspiring stories of those who have overcome Diabetes will keep you motivated