I Need Insulin
My doctor is insisting on Insulin, what do I need to know ?
Insulin is produced in our body naturally by the pancreatic cells and helps the body in converting sugar into energy. When our body produces insufficient or no insulin then doctors recommend taking Insulin additionally, to ensure body metabolises carbohydrates into sugar, and sugar does not accumulate for a prolonged period of time in the form of blood glucose.
There are myths associated with taking Insulin, read below to find out the most frequently asked questions by people living with diabetes.
I have been asked by my doctor to take Insulin, is my Diabetes getting worse ?
Taking Insulin does not necessarily mean that your Diabetes is getting worse. To control your high blood glucose levels your doctor may prescribe Insulin therapy. By not taking the Insulin therapy you may further develop Diabetes-related complications such as Glaucoma in the eyes and malfunctioning of the kidneys or the liver, neuropathy, foot problems, nerve related issues etc. People with Type 2 Diabetes often use combined therapy of medicine and Insulin to keep their sugar levels in control.
Will injecting Insulin be painful ?
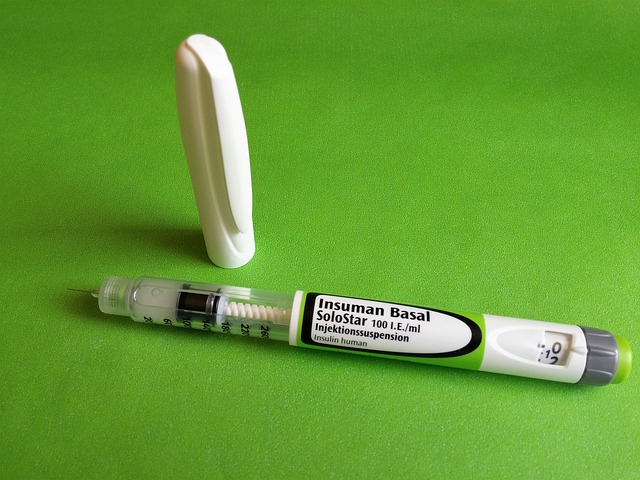
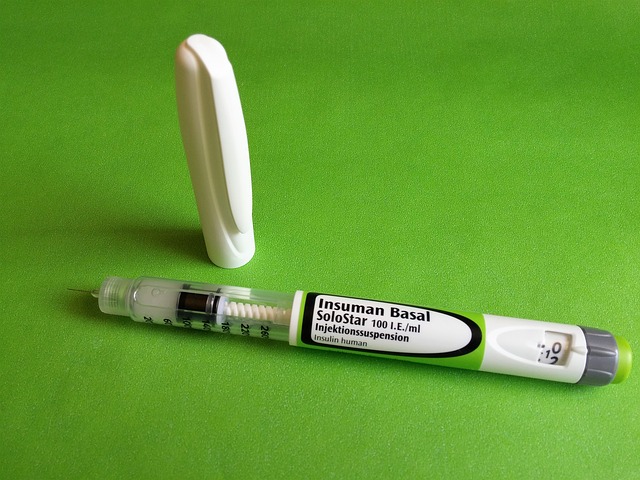
Injecting Insulin is not as painful as you may think. Your doctor will direct you how to inject Insulin in the right way and painlessly. Insulin should be given in the areas where one has more flab and less muscle. There are many new types of syringes which are thinner and painless to use, so this should not be a cause for worry.
Once I begin Insulin, will I have to take it for the rest of my life ?
The answer to this question is different for different types of Diabetes. For people living with Type 1 Diabetes this is true; however, for people with Type 2 Diabetes, studies have shown that taking medication on time, physical exercises and diet control can lead to reversal of the condition. Some people simply do not want to start Insulin because of the fear of having to take it forever. However studies have revealed that once the blood glucose levels are under control, patients have been able to switch back to oral medication and no longer have to depend on Insulin.
Travelling with Insulin is tedious, can I miss my injections ?
Doctors all round the world strongly recommend that people who are Insulin dependent must not miss any injections. If you miss your regular dose, it will disrupt the ground you have gained in Diabetes management and take you back to square one. Your blood sugar levels will shoot up and create an imbalance of toxins in the body, leading to further complications.
It is a good idea to make your own small back-pack where you could keep your syringes, Insulin, cotton, gauze and astringent handy. Insulin has to be kept in a cool place and, hence, sometimes needs to be refrigerated. If you are travelling, check with your pharmacist for new types of Insulin pens and cartridges, which might not need refrigeration.
What I can do as family/friend of a person living on Insulin ?
If your partner has Insulin-dependent Diabetes, we understand that you would have your own set of stresses that can be mentally and physically exhausting. You would need to be able to support your partner in different ways, such as establishing and maintaining a healthy diet and exercise routine, checking your partner for wounds that may be concerning, learning to give Insulin shots correctly and painlessly, as well as routinely check blood glucose levels.
There are quite a few things that you can do to help yourself and your partner. First and foremost, in order to support your partner in living with this condition, you need to take care of yourself, both mentally and physically. Establish a health plan for yourself, which will keep you in good shape to deal with the stresses that go along with Diabetes. It is even better if you can exercise together. Taking up meditation and yoga is also a very good way to reduce the impact of stress on your body.
You do not need to give up your life and pleasures in order to support your partner. For example, develop a balanced diet plan that takes care of your partner’s nutritional requirements, but do not forget to add your favourite dish to the equation!
Consult with your doctor to plan an evening out, away from the regular routine. Understand and follow the doctor’s instructions when it comes to dos and don’ts for eating and drinking on your evening out, and you will be fine.
Make sure to have a backup for yourself. As you support your partner in living with Diabetes, you need not give up your interests. Have family/friends provide you with backup whenever you need to step away for some time. This also takes care of the condition known as “compassion fatigue” in caregivers.
It is also good to have support of other people living with this condition just in case you yourself are under the weather for a couple of days.
To read more on Diabetes, click on the link below.