Just Detected

Being diagnosed with diabetes can be an overwhelming experience In fact, it can be a major life stress for many people. This is especially true as most chronic conditions and progressive diseases can prove to be quite challenging to manage emotionally.
If you or your family are feeling anxious and disheartened, you should know that it is natural to feel that way. You should also know that you are not alone, and that 70 million other people in India are living with Diabetes. This is a condition that needs to be “managed”.
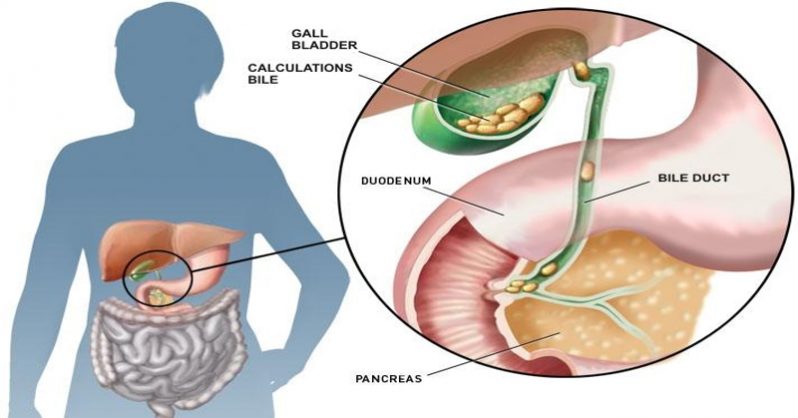
In brief, Diabetes is characterized by high blood glucose levels that result from defects in the body’s ability to produce enough insulin, and at times no insulin is produced at all. Insulin is required to remove sugars and toxins from our system, and when they do not get flushed out, they tend to accumulate, resulting in high blood glucose levels.
You will be happy to know there are countless cases of people who have reversed their condition simply by making changes in their daily lives, especially when it comes to food, exercise and stress management. With some precautions and care, we are confident that you too can be a winner.
Remember, with a clear plan, appropriate guidance, right (and on time) medications, timely tests and appropriate modifications to your lifestyle you can not only overcome your condition but stay on top of it. To know more, please refer to our Let’s Understand section
Remember, we are here to help you in your endeavour to stay focussed and on target!
Some quick tips that the American Diabetes Association and other bodies recommend that you should follow:
- Find a good doctor
- We recommend seeking the advice of a specialist, in this case an ‘endocrinologist’ or ‘diabetologist’ who can help and direct you with a constructive plan of action. Check with your doctor if you have to repeat your tests.
- Acquire as much information as you can
- An informed person can make better decisions. Therefore, it is essential for you to get to know more about food and other lifestyle changes that will help you manage better. Newly-diagnosed people are frequently advised to control blood sugar levels by following a healthy nutrition plan along with a regular exercise regime. To know more, read recommended diets and exercise plans for people living with diabetes.
- Seek help and support from your family
- Research suggests that with family support one can manage diabetes much more effectively than running self-managed programmes. Your partner, family, and friends play a huge role in motivating you and helping you adhere to your diabetes management programme.
- Make your own plan:
- As you may already know, food plays a very important role in diabetes management. An ideal diabetes meal plan consists of low carbs, low sugar, lean proteins and high fibre diet. You may choose from a wide variety of Diabetes meal plans available to you. Before you start following one, you are advised to check with your doctor or dietician regarding the amount of calories you need to take in a day/week, according to your BMI and physical activity rate.
You may also seek a dietician’s advice to put together a plan that works best for you
- As you may already know, food plays a very important role in diabetes management. An ideal diabetes meal plan consists of low carbs, low sugar, lean proteins and high fibre diet. You may choose from a wide variety of Diabetes meal plans available to you. Before you start following one, you are advised to check with your doctor or dietician regarding the amount of calories you need to take in a day/week, according to your BMI and physical activity rate.
- Check on Alcohol and tobacco consumption
- Research suggests smoking may aggravate complications from Diabetes, such as heart diseases and may lead to nerve and kidney damage. It is, therefore, highly advisable to significantly limit or give up smoking.
Alcohol consumption can have a strong impact on your blood sugar levels, not to mention liver-related disorders. It is a good idea to take your doctor’s advice on whether you can consume alcohol, and how much. In any case, please remember to always eat a meal while consuming alcohol to prevent fluctuations or spiking of blood glucose levels.
- Research suggests smoking may aggravate complications from Diabetes, such as heart diseases and may lead to nerve and kidney damage. It is, therefore, highly advisable to significantly limit or give up smoking.
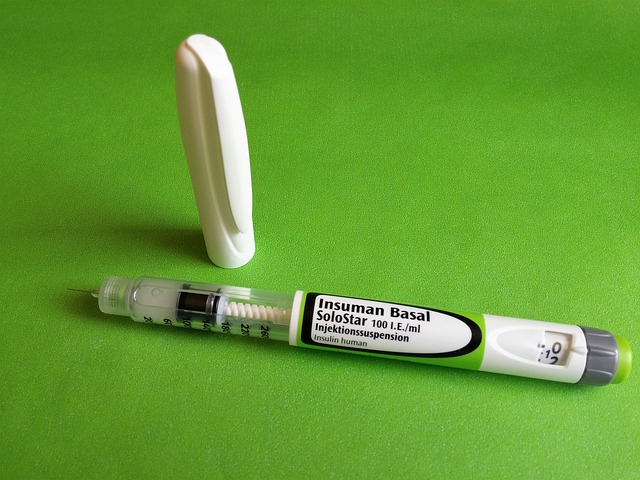
- Medicines – on time, every time!
- One of the most crucial aspects of Diabetes management is to take your medication regularly and avoiding skipping meals. The medical explanation is that medicines and food have a direct role in keeping “good control” of blood glucose levels.
If your doctor has advised you to take Insulin then please DO NOT skip your shots. Many people fear pain or scarring resulting from the Insulin shots, and the good news is that one can learn the right, less painful ways of taking Insulin. Refer to our “Insulin section” for more details.
In fact, in order to keep your blood glucose levels in control, you should eat small meals more frequently and consult a dietician to plan the best possible meal plan for you.
- One of the most crucial aspects of Diabetes management is to take your medication regularly and avoiding skipping meals. The medical explanation is that medicines and food have a direct role in keeping “good control” of blood glucose levels.
- Indulge yourself. Take extra care of your teeth to keep gum diseases at bay
- While it is true that you have to follow a strict plan, talk to your doctor about rewarding yourself once in a while.
However, do keep in mind the fact that you have to keep up with your basic health and hygiene requirements. Do brush your teeth at least twice a day, as people living with Diabetes tend to have frequently-returning gum infections. You should also floss your teeth once a week and see a dentist at least twice a year. Inform your dentist if your gums bleed or get swollen to have the concerns addressed at the earliest.
- While it is true that you have to follow a strict plan, talk to your doctor about rewarding yourself once in a while.
- Be careful about Wounds
- Take your wounds seriously, do go and see a doctor immediately if you feel your wounds are healing slowly, or not healing at all as high blood sugar can reduce blood flow, damage nerves and delay healing. It is essential to take care of your foot as minor cuts and blisters can lead to serious infections. Infact people living with Diabetes should also monitor for tingling or loss of sensation in the hands and feet.
- Last but not the least
- With a strong determination and sincere effort, one can easily control Diabetes and enjoy living life like never before.
Join the support community for family and friends of people living with Diabetes, a unique platform to share, help and bring a change in the lives of families and people living with Diabetes.
- With a strong determination and sincere effort, one can easily control Diabetes and enjoy living life like never before.
What can I do as a family/friend of a newly diagnosed loved one ?
As a partner or caregiver, it is understandable that your feel anxious and concerned on hearing the diagnosis of Diabetes.
Please be assured that there is no cause for concern as this is a condition that can be managed with a little care and diligence. You may need to play a pivotal role in the management of the condition for your partner or a loved one and therefore, you would need to be supporting and considerate. Research points to high success rates for diabetics that have had the support of a spouse or family member.
- No need to panic
- While Diabetes is considered a lifelong “chronic” condition, there is no need to panic as it can be managed with lifestyle and diet changes. Please be caring and supportive as your partner/family member may have to depend on you to make the required changes and live a long and healthy life
- Participate
- It is a good idea to actively participate in your partner’s plans and health goals. By working as a team your support is implicit. Set reminders to take medication on time, learn how to inject insulin, figure out what food items work and what don’t. Set realistic goals, and learn the fine art of encouraging without nagging.
- De-stress yourself
- Diabetes can impact the whole family and not just the person living with the condition. In order to avoid the caregiver fatigue syndrome, it is a good idea to spend some time for you. Take timeout to pursue your own goals and keep up with your friends and associates outside of the Diabetic circle.
To read more on Diabetes, click on the link below.